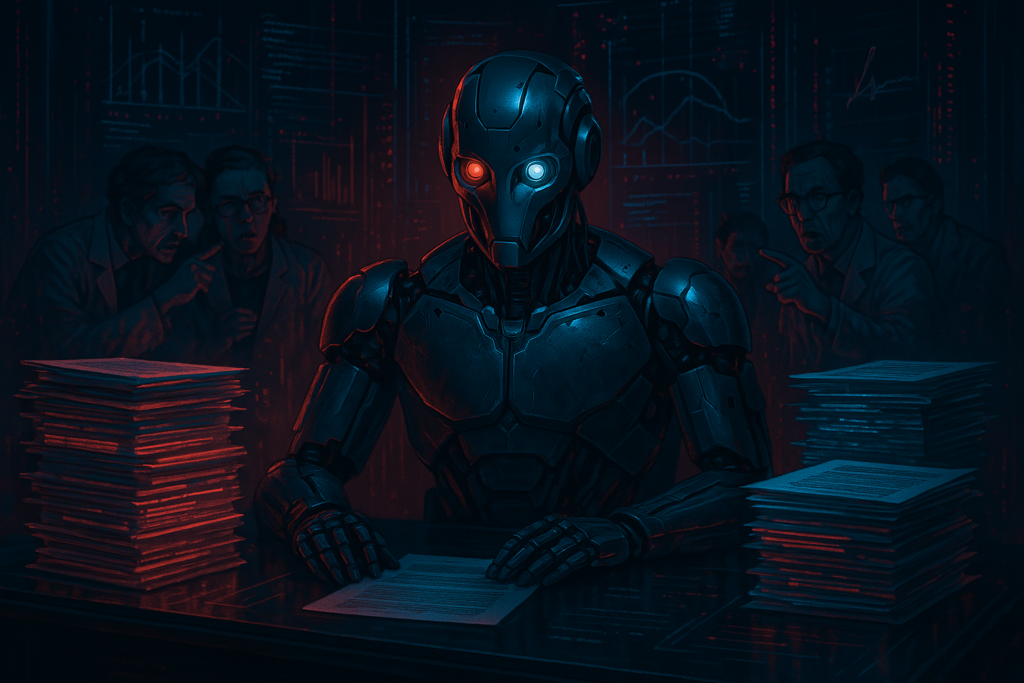
Artificial Intelligence: Addressing Clinical Trials’ Greatest Challenges
Modern medicine is a marvel, with previously unimaginable cures and treatments now widely available. Think of advanced medical devices such as implantable defibrillators that help regulate heart rhythm and reduce the risk of cardiac arrest. Such breakthroughs would not have been possible without clinical trials – the rigorous research that evaluates the effects of medical […] The post Artificial Intelligence: Addressing Clinical Trials’ Greatest Challenges appeared first on Unite.AI.


Modern medicine is a marvel, with previously unimaginable cures and treatments now widely available. Think of advanced medical devices such as implantable defibrillators that help regulate heart rhythm and reduce the risk of cardiac arrest.
Such breakthroughs would not have been possible without clinical trials – the rigorous research that evaluates the effects of medical interventions on human participants.
Unfortunately, the clinical trial process has become slower and more expensive over time. In fact, only one in seven drugs that enter phase I trials – the first stage of testing for safety – are eventually approved. It currently takes, on average, nearly a billion dollars in funding and a decade of work to bring one new medicinal product to market.
Half of this time and money is spent on clinical trials, which face mounting hurdles, including recruitment inefficiencies, limited diversity, and patient inaccessibility. Consequently, drug discovery slows, and costs continue to rise. Fortunately, recent advancements in Artificial Intelligence have the potential to break the trend and transform drug development for the better.
From models that predict complex protein interactions with remarkable precision, to AI-powered lab assistants streamlining routine tasks, AI-driven innovation is already reshaping the pharmaceutical landscape. Adopting new AI capabilities to address clinical trial barriers can enhance the trial process for patients, physicians and BioPharma, paving the way for new impactful drugs and potentially better health outcomes for patients.
Barriers to Drug Development
Drugs in development face numerous challenges throughout the clinical trial process, resulting in alarmingly low approval rates from regulatory bodies like the U.S. Food and Drug Administration (FDA). As a result, many investigational medicines never reach the market. Key challenges include trial design setbacks, low patient recruitment, and limited patient accessibility and diversity – issues that compound one another and hinder progress and equity in drug development.
1. Trial Site Selection Challenges
The success of a clinical trial largely depends on whether the trial sites—typically hospitals or research centers— can recruit and enroll sufficient eligible study population. Site selection is traditionally based on several overlapping factors, including historical performance in previous trials, local patient population and demographics, research capabilities and infrastructure, available research staff, duration of the recruitment period, and more.
On its own, each criterion is quite straightforward, but the process of gathering data around each is fraught with challenges and the results may not reliably indicate whether the site is appropriate for the trial. In some cases, data may simply be outdated, or incomplete, especially if validated on only a small sample of studies.
The data that helps determine site selection also comes from different sources, such as internal databases, subscription services, vendors, or Contract Research Organizations, which provide clinical trial management services. With so many converging factors, aggregating and assessing this information can be confusing and convoluted, which in some cases can lead to suboptimal decisions on trial sites. As a result, sponsors – the organizations conducting the clinical trial – may over or underestimate their ability to recruit patients in trials, leading to wasted resources, delays and low retention rates.
So, how can AI help with curating trial site selection?
By training AI models with the historical and real-time data of potential sites, trial sponsors can predict patient enrollment rates and a site’s performance – optimizing site allocation, reducing over- or under-enrollment, and improving overall efficiency and cost. These models can also rank potential sites by identifying the best combination of site attributes and factors that align with study objectives and recruitment strategies.
AI models trained with a mix of clinical trial metadata, medical and pharmacy claims data, and patient data from membership (primary care) services can also help identify clinical trial sites that will provide access to diverse, relevant patient populations. These sites can be centrally located for underrepresented groups or even take place in popular sites within the community such as barber shops, or faith-based and community centers, helping to address both the barriers of patient accessibility and lack of diversity.
2. Low Patient Recruitment
Patient recruitment remains one of the biggest bottlenecks in clinical trials, consuming up to one-third of a study’s duration. In fact, one in five trials fail to recruit the required number of participants. As trials become more complex – with additional patient touchpoints, stricter inclusion and exclusion criteria, and increasingly sophisticated study designs – recruitment challenges continue to grow. Not surprisingly, research links the rise in protocol complexity to declining patient enrollment and retention rates.
On top of this, strict and often complex eligibility criteria, designed to ensure participant safety and study integrity, often limit access to treatment and disproportionately exclude certain patient populations, including older adults and racial, ethnic, and gender minorities. In oncology trials alone, an estimated 17–21% of patients are unable to enroll due to restrictive eligibility requirements.
AI is poised to optimize patient eligibility criteria and recruitment. While recruitment has traditionally required that physicians manually screen patients – which is incredibly time consuming – AI can efficiently and effectively match patient profiles against suitable trials.
For example, machine learning algorithms can automatically identify meaningful patterns in large datasets, such as electronic health records and medical literature, to improve patient recruitment efficiency. Researchers have even developed a tool that uses large language models to rapidly review candidates on a large scale and help predict patient eligibility, reducing patient screening time by over 40%.
Healthtech companies adopting AI are also developing tools that help physicians to quickly and accurately determine eligible trials for patients. This supports recruitment acceleration, potentially allowing trials to start sooner and therefore providing patients with earlier access to new investigational treatments.
3. Patient Accessibility and Limited Diversity
AI can play a critical role in improving access to clinical trials, especially for patients from underrepresented demographic groups. This is important, as inaccessibility and limited diversity not only contribute to low patient recruitment and retention rates but also lead to inequitable drug development.
Consider that clinical trial sites are generally clustered in urban areas and large academic centers. The outcome is that communities in rural or underserved areas are often unable to access these trials. Financial burdens such as treatment costs, transportation, childcare, and the cost of missing work compound the barriers to trial participation and are more pronounced in ethnic and racial minorities and groups with lower-than-average socioeconomic status.
As a result, racial and ethnic minority groups represent as little as 2% of patients in US clinical trials, despite making up 39% of the national population. This lack of diversity poses a significant risk in relation to genetics, which vary across racial and ethnic populations and can influence adverse drug responses. For instance, Asians, Latinos, and African Americans with atrial fibrillation (abnormal heart rhythms related to heart-related complications) who take warfarin, a medication that prevents blood clots, have a higher risk of brain bleeds compared to those of European ancestry.
Greater representation in clinical trials is therefore essential in helping researchers develop treatments that are both effective and safe for diverse populations, ensuring that medical advancements benefit everyone – not just select demographic groups.
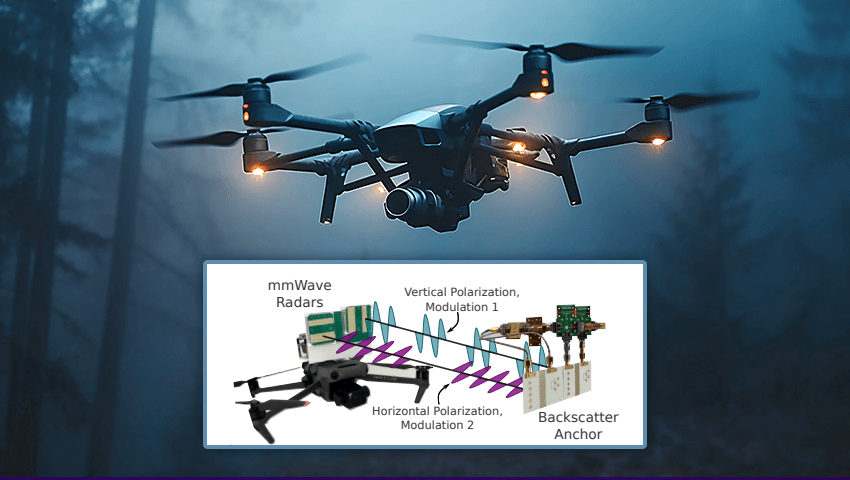
AI can help clinical trial sponsors tackle these challenges by facilitating decentralized trials – moving trial activities to remote and alternative locations, rather than collecting data at a traditional clinical trial site.
Decentralized trials often utilize wearables, which collect data digitally and use AI-powered analytics to summarize relevant anonymized information regarding trial participants. Combined with electronic check-ins, this hybrid approach to clinical trial enactment can eliminate geographical barriers and transportation burdens, making trials accessible to a broader range of patients.
Smarter Trials Make Smarter Treatments
Clinical trials are yet another sector which stands to be transformed by AI. With its ability to analyze large datasets, identify patterns, and automate processes, AI can provide holistic and robust solutions to today’s hurdles – optimizing trial design, enhancing patient diversity, streamlining recruitment and retention, and breaking down accessibility barriers.
If the healthcare industry continues to adopt AI-powered solutions, the future of clinical trials has the potential to become more inclusive, patient-centered, and innovative. Embracing these technologies isn’t just about keeping up with modern trends – it’s about creating a clinical research ecosystem that accelerates drug development and delivers more equitable healthcare outcomes for all.
The post Artificial Intelligence: Addressing Clinical Trials’ Greatest Challenges appeared first on Unite.AI.

































































![Lowest Prices Ever: Apple Pencil Pro Just $79.99, USB-C Pencil Only $49.99 [Deal]](https://www.iclarified.com/images/news/96863/96863/96863-640.jpg)
![Apple Releases iOS 18.4 RC 2 and iPadOS 18.4 RC 2 to Developers [Download]](https://www.iclarified.com/images/news/96860/96860/96860-640.jpg)
































































































































































![[The AI Show Episode 141]: Road to AGI (and Beyond) #1 — The AI Timeline is Accelerating](https://www.marketingaiinstitute.com/hubfs/ep%20141.1.png)
![[The AI Show Episode 140]: New AGI Warnings, OpenAI Suggests Government Policy, Sam Altman Teases Creative Writing Model, Claude Web Search & Apple’s AI Woes](https://www.marketingaiinstitute.com/hubfs/ep%20140%20cover.png)
![[The AI Show Episode 139]: The Government Knows AGI Is Coming, Superintelligence Strategy, OpenAI’s $20,000 Per Month Agents & Top 100 Gen AI Apps](https://www.marketingaiinstitute.com/hubfs/ep%20139%20cover-2.png)



















































































![From broke musician to working dev. How college drop-out Ryan Furrer taught himself to code [Podcast #166]](https://cdn.hashnode.com/res/hashnode/image/upload/v1743189826063/2080cde4-6fc0-46fb-b98d-b3d59841e8c4.png?#)


![[FREE EBOOKS] The Ultimate Linux Shell Scripting Guide, Artificial Intelligence for Cybersecurity & Four More Best Selling Titles](https://www.javacodegeeks.com/wp-content/uploads/2012/12/jcg-logo.jpg)


























.jpg?#)

.png?#)




















![Mini Review: Rendering Ranger: R2 [Rewind] (Switch) - A Novel Run 'N' Gun/Shooter Hybrid That's Finally Affordable](https://images.nintendolife.com/0e9d68643dde0/large.jpg?#)